Brain
Table of Contents
Introduction Brain-Gut Axis: The Unseen Connection
In the intricate tapestry of human biology, the brain and the gut, seemingly distant organs, are engaged in a profound and bidirectional communication network known as the brain-gut axis. This complex interplay, far beyond simple digestion, profoundly influences our physical and, crucially, our mental health. The food we consume is not just fuel for our bodies; it acts as a powerful modulator of this axis, impacting everything from our mood and cognition to our stress response and susceptibility to mental disorders.
This comprehensive guide delves deep into the fascinating world of the brain-gut axis, exploring the intricate mechanisms through which nutrition exerts its influence on our psychological well-being. We will unravel the science behind this connection, examine the role of the gut microbiome, identify key nutrients and dietary patterns that support mental health, and provide practical strategies for leveraging this knowledge to optimize our emotional and cognitive states.
Understanding the Brain-Gut Axis: A Two-Way Street
The brain-gut axis is not a one-way street; it involves a sophisticated bidirectional communication system that integrates neural, hormonal, and immunological signaling pathways. This intricate dialogue ensures that the brain influences gut function, and conversely, the gut profoundly impacts brain activity.
1. The Neural Pathway: The Vagus Nerve – The Superhighway of Communication
The vagus nerve, the longest cranial nerve in the body, serves as the primary neural pathway connecting the brain and the gut. This “wandering nerve” extends from the brainstem down to the abdomen, transmitting signals in both directions.
- Brain to Gut: Stress, anxiety, and even thoughts can trigger signals along the vagus nerve, influencing gut motility, secretion, and even the composition of the gut microbiome. This is why stress can manifest as digestive issues like irritable bowel syndrome (IBS).
- Gut to Brain: Sensory neurons in the gut lining detect changes in the gut environment, such as the presence of specific nutrients, microbial metabolites, or inflammatory molecules. These signals are then relayed to the brain via the vagus nerve, influencing mood, cognition, and behavior.
Quote: “The gut is the second brain.” – Michael Gershon, MD, author of “The Second Brain”
2. The Hormonal Pathway: Chemical Messengers of Influence
The gut produces a vast array of hormones that can enter the bloodstream and influence brain function. Conversely, the brain releases hormones that can impact gut physiology.
- Gut Hormones Affecting the Brain:
- Serotonin: While primarily known as a neurotransmitter in the brain regulating mood, sleep, and appetite, a significant majority (around 90%) of the body’s serotonin is produced in the gut. Gut bacteria play a crucial role in its synthesis.
- Dopamine: Another key neurotransmitter involved in pleasure, motivation, and reward, dopamine production is also influenced by gut health.
- Ghrelin and Leptin: These hormones, primarily involved in appetite regulation, also have effects on mood and cognitive function. Ghrelin (“hunger hormone”) can increase anxiety, while leptin (“satiety hormone”) has been linked to reduced depression in some studies.
- Short-Chain Fatty Acids (SCFAs): Produced by the fermentation of dietary fiber by gut bacteria, SCFAs like butyrate, acetate, and propionate can cross the blood-brain barrier and exert neuroprotective and mood-regulating effects.
- Brain Hormones Affecting the Gut:
- Cortisol: The primary stress hormone released by the adrenal glands in response to stress can significantly impact gut motility, permeability, and the gut microbiome composition. Chronic stress and elevated cortisol levels are often linked to digestive issues.
Comparison Table: Neural vs. Hormonal Communication
| Feature | Neural Pathway (Vagus Nerve) | Hormonal Pathway (Gut Hormones) |
|---|---|---|
| Speed | Fast (electrical signals) | Slower (chemical signals) |
| Specificity | Targeted communication | Broader systemic effects |
| Primary Mediator | Vagus nerve fibers | Gut-derived hormones |
| Examples | Stress-induced IBS, gut signals affecting mood | Serotonin production, cortisol impact on gut |
3. The Immunological Pathway: Inflammation and Mental Health
The gut harbors a vast and complex ecosystem of microorganisms, collectively known as the gut microbiome. This intricate community plays a vital role in digestion, nutrient absorption, and the development and regulation of the immune system. Disruptions in the gut microbiome, known as dysbiosis, can lead to increased intestinal permeability (“leaky gut”), allowing inflammatory molecules to enter the bloodstream and potentially reach the brain.
- Gut Microbiome and Inflammation: An imbalance in the gut microbiome can favor the growth of pro-inflammatory bacteria, leading to chronic low-grade inflammation throughout the body, including the brain (neuroinflammation). Neuroinflammation has been implicated in the pathogenesis of various mental disorders, including depression, anxiety, and neurodegenerative conditions.
- Microbiota-Gut-Brain Axis: The gut microbiome actively communicates with the brain through various mechanisms, including the production of neurotransmitters, SCFAs, and other metabolites that can influence brain function and behavior.
List: Key Mechanisms of Brain-Gut Axis Communication
- Vagal nerve signaling: Direct neural communication.
- Gut hormone release: Endocrine signaling influencing brain function.
- Production of neurotransmitters in the gut: Local and systemic effects.
- Short-chain fatty acid (SCFA) production: Metabolic signaling impacting brain health.
- Immune system modulation: Gut microbiome influences systemic and neuroinflammation.
- Enteric nervous system (ENS): The “second brain” within the gut, communicating locally and with the central nervous system.
The Gut Microbiome: A Symphony of Microbes and Mental Well-being
The gut microbiome, comprising trillions of bacteria, fungi, viruses, and other microorganisms, is increasingly recognized as a key player in the brain-gut axis and a significant modulator of mental health.
1. Diversity is Key: A Balanced Ecosystem
A diverse and balanced gut microbiome is generally associated with better physical and mental health. Factors like diet, lifestyle, stress, and antibiotic use can significantly impact the diversity and composition of this microbial community.
2. The Gut Microbiome and Neurotransmitter Production:
Gut bacteria can directly and indirectly influence the production of neurotransmitters that are crucial for mental well-being:
- Serotonin: Certain bacteria can synthesize serotonin precursors.
- Gamma-aminobutyric acid (GABA): Some bacterial species produce GABA, an inhibitory neurotransmitter with calming effects.
- Brain-Derived Neurotrophic Factor (BDNF): Gut bacteria can influence the production of BDNF, a protein essential for neuronal growth, survival, and plasticity, which is often reduced in individuals with depression and anxiety.
3. The Gut Microbiome and the Immune System:
The gut microbiome plays a critical role in educating and regulating the immune system. A healthy microbiome helps to maintain a balance between pro-inflammatory and anti-inflammatory responses. Dysbiosis can disrupt this balance, leading to increased inflammation that can impact brain function.
4. The Gut Microbiome and the Stress Response:
The gut microbiome can influence the hypothalamic-pituitary-adrenal (HPA) axis, the body’s primary stress response system. Dysbiosis has been linked to an overactive HPA axis and increased susceptibility to stress-related mental health issues.
Insight: Research suggests that specific strains of beneficial bacteria, known as psychobiotics, may have direct positive effects on mental health by influencing neurotransmitter production, reducing inflammation, and modulating the stress response.
Table: Impact of Gut Microbiome on Mental Health
| Mechanism | Impact on Mental Health |
|---|---|
| Neurotransmitter Production | Influences mood, sleep, anxiety, and cognition. |
| Immune System Modulation | Affects inflammation levels, potentially contributing to or protecting against mental disorders. |
| HPA Axis Regulation | Influences stress response and resilience. |
| Production of SCFAs | Provides energy for gut cells, reduces inflammation, and may have direct neuroprotective effects. |
| Modulation of Brain Function | Emerging evidence suggests direct influence on brain regions involved in emotion and cognition. |
Nutrition’s Profound Impact on the Brain-Gut Axis and Mental Health
The food we consume provides the building blocks for our brain, fuels our gut microbiome, and directly influences the communication pathways of the brain-gut axis. Therefore, nutrition plays a pivotal role in shaping our mental well-being.
1. The Role of Macronutrients:
- Complex Carbohydrates: Provide a steady release of glucose, the brain’s primary energy source. They also feed beneficial gut bacteria, promoting the production of SCFAs. Examples include whole grains, fruits, vegetables, and legumes.
- Healthy Fats: Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, have anti-inflammatory properties and are crucial for brain structure and function. They may also positively influence the gut microbiome.
- Lean Protein: Provides amino acids, the precursors for neurotransmitters like serotonin and dopamine. Sources include fish, poultry, beans, lentils, tofu, and eggs.
2. The Power of Micronutrients:
Vitamins and minerals are essential for various biochemical processes in the brain and gut, including neurotransmitter synthesis, enzyme function, and immune regulation. Deficiencies in certain micronutrients have been linked to an increased risk of mental health disorders.
- B Vitamins: Crucial for energy production and nerve function. Folate (B9) and vitamin B12 are particularly important for mood regulation and cognitive function.
- Vitamin D: Plays a role in brain development and function, and deficiency has been linked to depression.
- Magnesium: Involved in hundreds of enzymatic reactions, including those related to mood regulation and stress response.
- Zinc: Essential for neurotransmitter function and immune health.
- Iron: Crucial for oxygen transport to the brain; deficiency can lead to fatigue and cognitive impairment.
3. The Gut Microbiome’s Best Friends: Fiber and Fermented Foods:
- Dietary Fiber: Acts as a prebiotic, feeding beneficial gut bacteria and promoting their growth and diversity. Different types of fiber support different microbial communities. Sources include fruits, vegetables, whole grains, and legumes.
- Fermented Foods: Contain live beneficial bacteria (probiotics) that can help to diversify and balance the gut microbiome. Examples include yogurt (with live and active cultures), kefir, sauerkraut, kimchi, kombucha, and tempeh.
4. The Impact of Processed Foods and Unhealthy Fats:
Diets high in processed foods, refined sugars, and unhealthy fats (saturated and trans fats) can negatively impact both the brain and the gut microbiome.
- Inflammation: These dietary patterns can promote inflammation in the gut and systemically, potentially contributing to neuroinflammation.
- Gut Dysbiosis: They can favor the growth of less beneficial bacteria and reduce microbial diversity.
- Blood Sugar Imbalances: Rapid spikes and crashes in blood sugar can affect mood and energy levels.
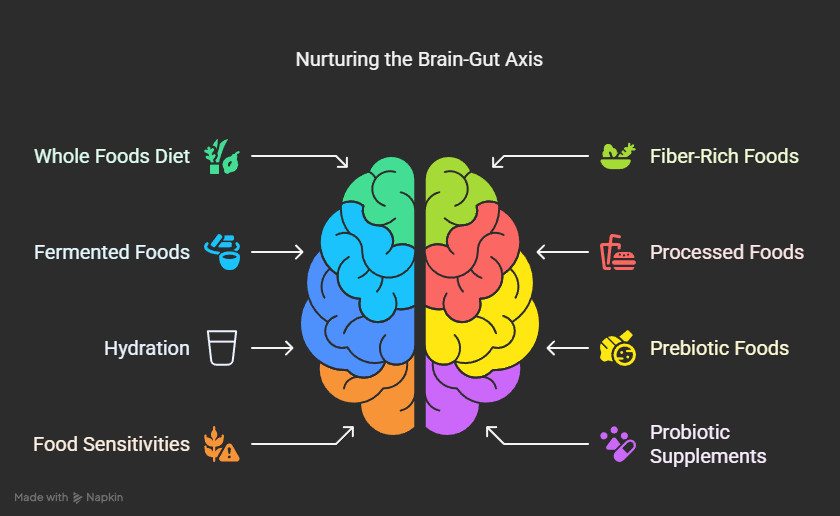
Tips for Nurturing Your Brain-Gut Axis and Mental Health Through Nutrition:
- Embrace a Whole Foods Diet: Focus on unprocessed, nutrient-dense foods like fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Prioritize Fiber-Rich Foods: Include a variety of fruits, vegetables, legumes, and whole grains to feed your beneficial gut bacteria. Aim for at least 25-30 grams of fiber per day.
- Incorporate Fermented Foods: Regularly consume fermented foods to introduce beneficial bacteria to your gut.
- Limit Processed Foods, Sugary Drinks, and Unhealthy Fats: These can disrupt your gut microbiome and promote inflammation.
- Stay Hydrated: Adequate water intake is essential for overall health and optimal gut function.
- Consider Prebiotic-Rich Foods: Onions, garlic, asparagus, bananas, and oats contain prebiotics that nourish beneficial gut bacteria.
- Be Mindful of Food Sensitivities: Identify and avoid foods that trigger digestive issues, as these can contribute to inflammation and impact the brain-gut axis.
- Consider a High-Quality Probiotic Supplement: If dietary changes are insufficient, a probiotic supplement (after consulting a healthcare professional) may be beneficial for supporting gut health. Choose strains with evidence-based benefits for mood and anxiety.
- Manage Stress: Chronic stress can negatively impact the gut microbiome. Incorporate stress-reducing practices like mindfulness, yoga, or meditation.
- Get Enough Sleep: Adequate sleep is crucial for both brain and gut health.
- Engage in Regular Exercise: Physical activity can positively influence the gut microbiome and reduce inflammation.
- Listen to Your Gut: Pay attention to how different foods make you feel, both physically and mentally.
Insight: The concept of nutritional psychiatry is an emerging field that focuses on the use of dietary interventions to prevent and treat mental health disorders. It emphasizes the crucial role of nutrition in modulating the brain-gut axis.
Quotes on the Brain-Gut Connection:
- “All disease begins in the gut.” – Hippocrates (ancient Greek physician)
- “The gut is not just a digestive system; it’s a complex neuroendocrine organ that communicates extensively with the brain.” – Emeran Mayer, MD, gastroenterologist and author of “The Mind-Gut Connection”
- “Food isn’t just fuel. It’s information. It talks to your genes, it talks to your gut microbes, and it talks to your brain.” – Mark Hyman, MD, physician and author”
The Gut Microbiome and Specific Mental Health Conditions:
Research is increasingly uncovering the role of the gut microbiome in various mental health conditions:
- Depression: Studies have shown differences in the gut microbiome composition of individuals with depression compared to healthy controls. Certain bacterial species may be associated with increased risk, while others may have protective effects. Psychobiotics have shown promise in alleviating depressive symptoms in some studies.
- Anxiety: Similar to depression, alterations in the gut microbiome have been observed in individuals with anxiety disorders. The gut microbiome’s influence on the HPA axis and neurotransmitter production (like GABA) is thought to play a role.
- Autism Spectrum Disorder (ASD): Gut issues are common in individuals with ASD, and research suggests a potential link between gut microbiome composition and ASD-related behaviors.
- Attention-Deficit/Hyperactivity Disorder (ADHD): Emerging research is exploring the connection between the gut microbiome and ADHD symptoms, particularly related to inflammation and neurotransmitter pathways.
- Schizophrenia: Some studies have found alterations in the gut microbiome of individuals with schizophrenia, suggesting a potential role in the development or progression of the disorder.
Caution: While research in this area is promising, it is still evolving. Nutritional interventions should be considered as part of a holistic approach to mental health and always discussed with a healthcare professional.
Comparison Table: Dietary Factors and Their Impact on Mental Health
| Dietary Factor | Potential Positive Impact on Mental Health | Potential Negative Impact on Mental Health |
|---|---|---|
| Whole Foods | Provides essential nutrients for brain function, supports a healthy gut microbiome, reduces inflammation. | Absence can lead to nutrient deficiencies and increased risk of mental health issues. |
| Dietary Fiber | Feeds beneficial gut bacteria, promotes SCFA production, supports gut health, may reduce inflammation. | Low intake can lead to gut dysbiosis and reduced SCFA production. |
| Fermented Foods | Introduces beneficial bacteria to the gut, potentially improving gut microbiome diversity and function. | May not be suitable for everyone, especially those with histamine intolerance. |
| Omega-3 Fatty Acids | Anti-inflammatory properties, crucial for brain structure and function, may positively influence gut microbiome. | Low intake may be associated with increased risk of mood disorders. |
| B Vitamins | Essential for energy production, nerve function, and neurotransmitter synthesis. | Deficiencies (e.g., folate, B12) linked to mood disorders and cognitive impairment. |
| Processed Foods | Generally low in nutrients and high in unhealthy fats, sugars, and additives. | Can promote inflammation, gut dysbiosis, blood sugar imbalances, and potentially increase the risk of mental health issues. |
| Refined Sugars | Can cause rapid blood sugar spikes and crashes, may negatively impact mood and energy levels, can feed less beneficial gut bacteria. | High intake linked to increased risk of depression and anxiety. |
| Unhealthy Fats (Saturated & Trans) | Can promote inflammation and negatively impact cardiovascular health, potentially indirectly affecting brain health. | High intake may be associated with increased risk of cognitive decline and mood disorders. |
The Future of Nutritional Psychiatry: Personalized Approaches
The field of nutritional psychiatry is moving towards more personalized approaches, recognizing that individual responses to dietary interventions can vary based on genetics, gut microbiome composition, lifestyle, and other factors.
- Personalized Nutrition: Tailoring dietary recommendations based on an individual’s unique biological profile, including their gut microbiome.
- Targeted Probiotics: Developing specific probiotic strains or combinations of strains to address particular mental health symptoms.
- Fecal Microbiota Transplantation (FMT): In some cases, transferring fecal matter from a healthy donor to a recipient with a dysbiotic gut microbiome is being explored as a potential treatment for certain conditions.
FAQs: Your Questions Answered
Q: Can diet alone cure mental illness?
A: While nutrition plays a crucial role in supporting mental health, it is generally not a standalone cure for diagnosed mental illnesses. Mental health conditions are complex and often require a multi-faceted approach involving therapy, medication, and lifestyle interventions, including nutrition.
Q: How long does it take to see the effects of dietary changes on mental health?
A: The timeline can vary depending on the individual, the specific dietary changes, and the severity of any mental health symptoms. Some people may notice improvements in mood and energy levels within a few weeks, while more significant changes in gut microbiome composition and mental well-being may take several months. Consistency is key.
Q: What are some signs of an unhealthy gut that might impact mental health?
A: Signs of an unhealthy gut can include:
* Frequent digestive issues like bloating, gas, constipation, or diarrhea.
* Food sensitivities or intolerances.
* Autoimmune conditions.
* Skin problems like eczema.
* Fatigue.
* Difficulty concentrating or “brain fog.”
* Mood swings or increased anxiety.
Q: Can stress directly impact my gut health and mental well-being?
A: Absolutely. The brain-gut axis is highly responsive to stress. Chronic stress can disrupt the gut microbiome, increase intestinal permeability, and trigger inflammatory responses, all of which can negatively impact mental health. Managing stress through techniques like mindfulness, exercise, and adequate sleep is crucial for both gut and brain health.
Q: Are there specific foods that are particularly good for mental health?
A: While a holistic dietary approach is most beneficial, certain foods stand out for their positive impact on the brain-gut axis and mental health:
* Fatty fish (salmon, mackerel, sardines): Rich in omega-3 fatty acids.
* Leafy green vegetables: High in folate and fiber.
* Berries: Packed with antioxidants and fiber.
* Nuts and seeds: Good sources of healthy fats, fiber, and magnesium.
* Legumes: Excellent source of fiber and prebiotics.
* Fermented foods (yogurt, kefir, kimchi): Provide beneficial probiotics.
* Whole grains: Offer sustained energy and fiber.
Q: Should I completely avoid certain food groups for better mental health?
A: Unless you have a diagnosed food allergy or intolerance, completely eliminating entire food groups is generally not recommended without professional guidance. A balanced and varied diet is usually the best approach. However, limiting processed foods, sugary drinks, and excessive amounts of unhealthy fats is generally beneficial for both physical and mental health.
Q: How can I find a healthcare professional who understands the brain-gut axis and nutritional psychiatry?
A: Look for professionals who specialize in integrative or functional medicine, nutritional psychiatry, or gut health. Registered dietitians with expertise in mental health or gastroenterology can also be valuable resources. You can search online directories or ask your primary care physician for recommendations.
Conclusion: Nourishing the Connection for a Healthier Mind
The brain-gut axis represents a fundamental connection in our biology, highlighting the profound influence of nutrition on our mental health. By understanding this intricate communication network and the vital role of the gut microbiome, we can make informed dietary choices that nourish both our bodies and our minds.
Embracing a whole foods diet rich in fiber, fermented foods, and essential nutrients, while limiting processed foods and unhealthy fats, can foster a healthy gut microbiome, reduce inflammation, and support optimal brain function. While nutrition is not a singular solution for mental illness, it serves as a powerful tool in promoting resilience, improving mood, and supporting overall psychological well-being.
As the field of nutritional psychiatry continues to evolve, personalized dietary interventions based on individual gut microbiome profiles and other biological factors hold immense promise for the future of mental health care. By recognizing and nurturing the brain-gut connection, we can empower ourselves to cultivate a healthier and happier life, one nourishing meal at a time.
Discover more from NutriIgnite UK
Subscribe to get the latest posts sent to your email.

Comments are closed.